| Date of Action |
Assembly Actions -
Lowercase Senate Actions - UPPERCASE |
|---|---|
| May 30, 2014 |
print number 2319a |
| May 30, 2014 |
amend and recommit to insurance |
| Jan 08, 2014 |
referred to insurance |
| Jan 15, 2013 |
referred to insurance |
Senate Bill S2319A
2013-2014 Legislative Session
Sponsored By
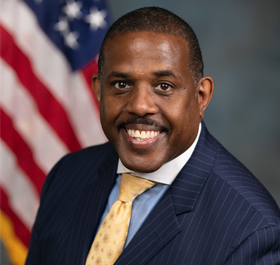
(R, C, IP) Senate District
Archive: Last Bill Status - In Senate Committee Insurance Committee
Actions
Bill Amendments
co-Sponsors
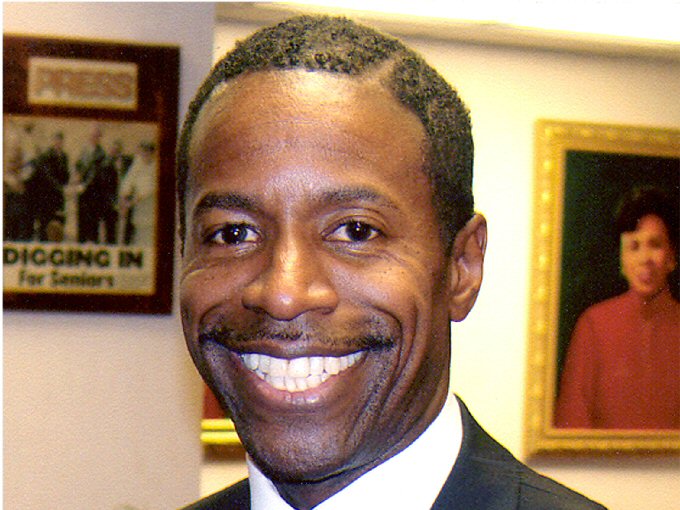
(D) 15th Senate District
(D) Senate District
(R) Senate District
(D) Senate District
2013-S2319 - Details
- See Assembly Version of this Bill:
- A1666
- Current Committee:
- Senate Insurance
- Law Section:
- Insurance Law
- Laws Affected:
- Amd §§3216, 4235, 4301 & 4322, Ins L
- Versions Introduced in Other Legislative Sessions:
-
2009-2010:
S4321, A8171
2011-2012: S4870, A187
2015-2016: S28, A1063
2017-2018: S5764, A569
2019-2020: S3751, A405
2021-2022: S3562, A594
2023-2024: S1470, A6345
2025-2026: S5045, A6484
2013-S2319 - Sponsor Memo
BILL NUMBER:S2319
TITLE OF BILL: An act to amend the insurance law, in relation to
physical therapy services
PURPOSE: To limit the imposition of co-payments for physical therapy
services to no more than twenty percent of the reimbursement to the
provider of care.
SUMMARY OF PROVISIONS:
Sections 1 through 5 prohibit payors from imposing costs on insureds
for the provision of physical therapy services in excess of 20 percent
of the reimbursement to the provider of care.
Section 6. Effective Date.
JUSTIFICATION: This bill will protect consumers by prohibiting plans
from inappropriately shifting the cost of physical therapy care to
consumers by limiting co-payments to no more than 20 percent of the
total reimbursement to the provider of care. Under existing law,
health plans must cover physical therapy services. Despite that
requirement, health plans have shifted the vast majority of the cost
of physical therapy services by imposing increasingly high co-payments
on consumers. Under certain health plans, co-payments for physical
therapy services have exceeded the reimbursement paid by the plan to
2013-S2319 - Bill Text download pdf
S T A T E O F N E W Y O R K
________________________________________________________________________
2319
2013-2014 Regular Sessions
I N S E N A T E
January 15, 2013
___________
Introduced by Sen. DeFRANCISCO -- read twice and ordered printed, and
when printed to be committed to the Committee on Insurance
AN ACT to amend the insurance law, in relation to physical therapy
services
THE PEOPLE OF THE STATE OF NEW YORK, REPRESENTED IN SENATE AND ASSEM-
BLY, DO ENACT AS FOLLOWS:
Section 1. Paragraph 23 of subsection (i) of section 3216 of the
insurance law, as added by chapter 593 of the laws of 2000, is amended
to read as follows:
(23) If a policy provides for reimbursement for physical and occupa-
tional therapy service which is within the lawful scope of practice of a
duly licensed physical or occupational therapist, an insured shall be
entitled to reimbursement for such service whether the said service is
performed by a physician or through a duly licensed physical or occupa-
tional therapist, provided however, that nothing contained herein shall
be construed to impair any terms of such policy including appropriate
utilization review and the requirement that said service be performed
pursuant to a medical order, or a similar or related service of a physi-
cian PROVIDED THAT SUCH TERMS SHALL NOT IMPOSE CO-PAYMENTS IN EXCESS OF
TWENTY PERCENT OF THE TOTAL REIMBURSEMENT TO THE PROVIDER OF CARE.
S 2. Subparagraph (A) of paragraph 1 of subsection (f) of section 4235
of the insurance law, as amended by chapter 219 of the laws of 2011, is
amended to read as follows:
(A) Any policy of group accident, group health or group accident and
health insurance may include provisions for the payment by the insurer
of benefits for expenses incurred on account of hospital, medical or
surgical care or physical and occupational therapy by licensed physical
and occupational therapists upon the prescription or referral of a
physician for the employee or other member of the insured group, the
employee's or member's spouse, the employee's or member's child or chil-
EXPLANATION--Matter in ITALICS (underscored) is new; matter in brackets
[ ] is old law to be omitted.
LBD03730-01-3
co-Sponsors
(D) 15th Senate District
(D) Senate District
(R) Senate District
(R, C) 60th Senate District
2013-S2319A (ACTIVE) - Details
- See Assembly Version of this Bill:
- A1666
- Current Committee:
- Senate Insurance
- Law Section:
- Insurance Law
- Laws Affected:
- Amd §§3216, 4235, 4301 & 4322, Ins L
- Versions Introduced in Other Legislative Sessions:
-
2009-2010:
S4321, A8171
2011-2012: S4870, A187
2015-2016: S28, A1063
2017-2018: S5764, A569
2019-2020: S3751, A405
2021-2022: S3562, A594
2023-2024: S1470, A6345
2025-2026: S5045, A6484
2013-S2319A (ACTIVE) - Sponsor Memo
BILL NUMBER:S2319A
TITLE OF BILL: An act to amend the insurance law, in relation to
physical therapy services
PURPOSE:
To limit the imposition of co-payments for physical therapy services
to no more than twenty percent of the reimbursement to the provider of
care.
SUMMARY OF PROVISIONS:
Sections 1 through 5 prohibit payors from imposing costs on insureds
for the provision of physical therapy services in excess of 20 percent
of the reimbursement to the provider of care.
Section 6. Effective Date.
JUSTIFICATION:
This bill will protect consumers by prohibiting plans from
inappropriately shifting the cost of physical therapy care to
consumers by limiting co-payments to no more than 20 percent of the
total reimbursement to the provider of care. Under existing law,
health plans must cover physical therapy services. Despite that
2013-S2319A (ACTIVE) - Bill Text download pdf
S T A T E O F N E W Y O R K
________________________________________________________________________
2319--A
2013-2014 Regular Sessions
I N S E N A T E
January 15, 2013
___________
Introduced by Sens. DeFRANCISCO, ADDABBO, AVELLA, BOYLE, GIPSON, GRISAN-
TI, HANNON, KENNEDY, LANZA, LATIMER, LIBOUS, MARCHIONE, MARTINS,
MAZIARZ, PARKER, PERKINS, RANZENHOFER, RITCHIE, ROBACH, SAMPSON,
SMITH, STAVISKY, TKACZYK, VALESKY, YOUNG -- read twice and ordered
printed, and when printed to be committed to the Committee on Insur-
ance -- recommitted to the Committee on Insurance in accordance with
Senate Rule 6, sec. 8 -- committee discharged, bill amended, ordered
reprinted as amended and recommitted to said committee
AN ACT to amend the insurance law, in relation to physical therapy
services
THE PEOPLE OF THE STATE OF NEW YORK, REPRESENTED IN SENATE AND ASSEM-
BLY, DO ENACT AS FOLLOWS:
Section 1. Paragraph 23 of subsection (i) of section 3216 of the
insurance law, as added by chapter 593 of the laws of 2000, is amended
to read as follows:
(23) If a policy provides for reimbursement for physical and occupa-
tional therapy service which is within the lawful scope of practice of a
duly licensed physical or occupational therapist, an insured shall be
entitled to reimbursement for such service whether the said service is
performed by a physician or through a duly licensed physical or occupa-
tional therapist, provided however, that nothing contained herein shall
be construed to impair any terms of such policy including appropriate
utilization review and the requirement that said service be performed
pursuant to a medical order, or a similar or related service of a physi-
cian PROVIDED THAT SUCH TERMS SHALL NOT IMPOSE CO-PAYMENTS IN EXCESS OF
TWENTY PERCENT OF THE TOTAL REIMBURSEMENT TO THE PROVIDER OF CARE.
S 2. Subparagraph (A) of paragraph 1 of subsection (f) of section 4235
of the insurance law, as amended by chapter 219 of the laws of 2011, is
amended to read as follows:
(A) Any policy of group accident, group health or group accident and
health insurance may include provisions for the payment by the insurer
EXPLANATION--Matter in ITALICS (underscored) is new; matter in brackets
[ ] is old law to be omitted.
LBD03730-03-4
Comments
Open Legislation is a forum for New York State legislation. All comments are subject to review and community moderation is encouraged.
Comments deemed off-topic, commercial, campaign-related, self-promotional; or that contain profanity, hate or toxic speech; or that link to sites outside of the nysenate.gov domain are not permitted, and will not be published. Attempts to intimidate and silence contributors or deliberately deceive the public, including excessive or extraneous posting/posts, or coordinated activity, are prohibited and may result in the temporary or permanent banning of the user. Comment moderation is generally performed Monday through Friday. By contributing or voting you agree to the Terms of Participation and verify you are over 13.
Create an account. An account allows you to sign petitions with a single click, officially support or oppose key legislation, and follow issues, committees, and bills that matter to you. When you create an account, you agree to this platform's terms of participation.