| Date of Action |
Assembly Actions -
Lowercase Senate Actions - UPPERCASE |
|---|---|
| Jan 08, 2020 |
referred to health |
| May 16, 2019 |
referred to health |
Senate Bill S5923
2019-2020 Legislative Session
Sponsored By
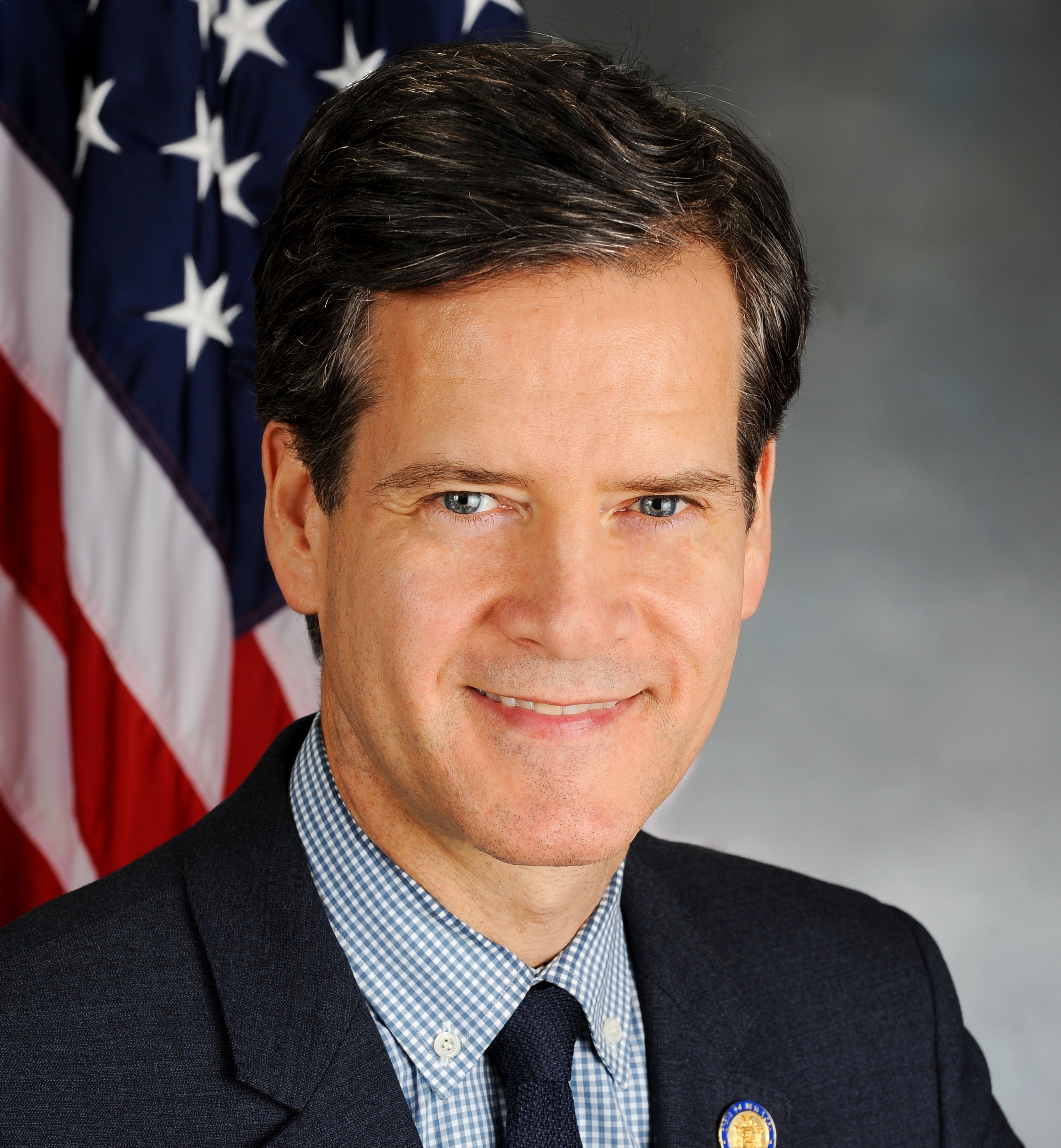
(D, WF) 33rd Senate District
Archive: Last Bill Status - In Senate Committee Health Committee
Actions
co-Sponsors
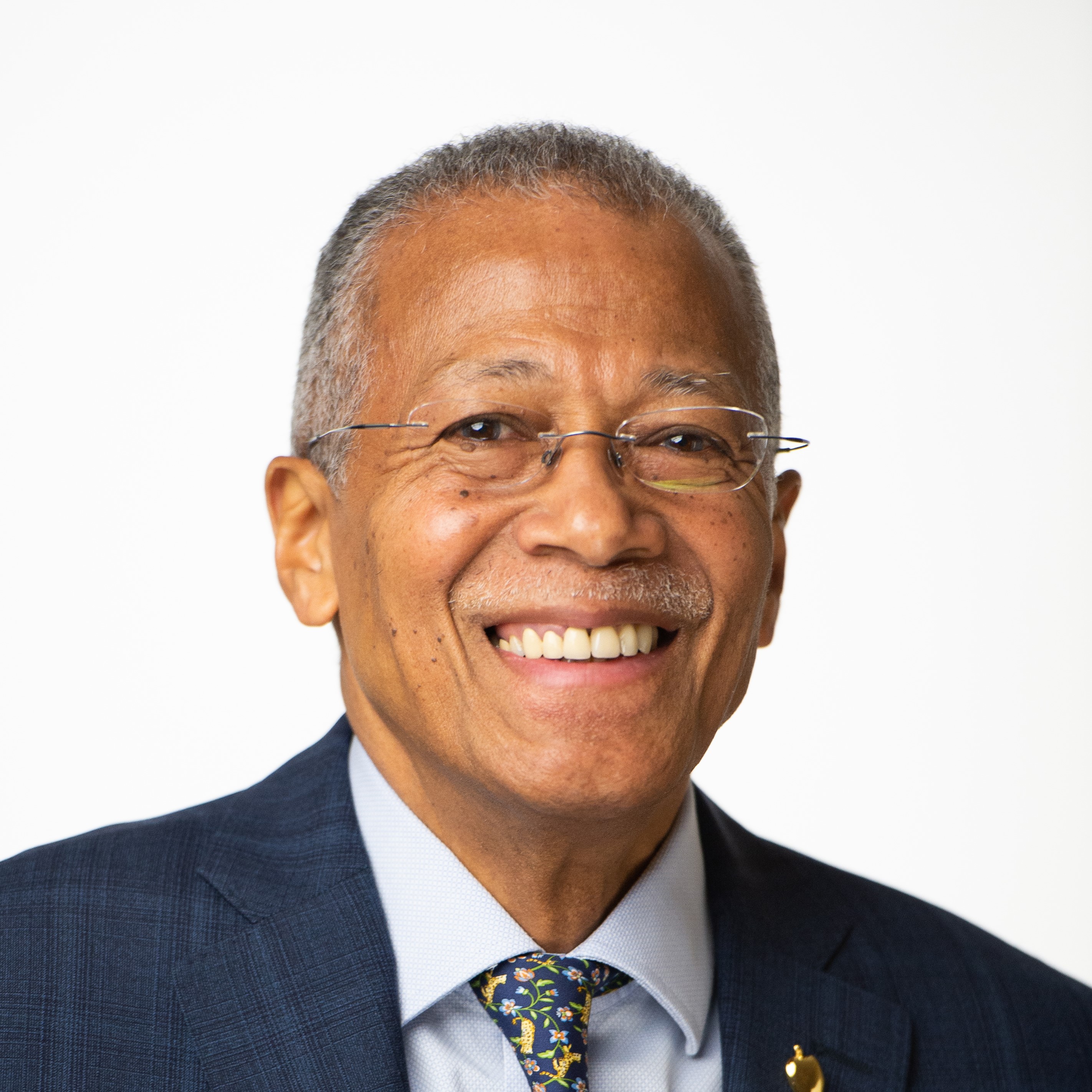
(D) 15th Senate District
(D) Senate District
(D) 14th Senate District
(D) Senate District
2019-S5923 (ACTIVE) - Details
- See Assembly Version of this Bill:
- A2795
- Current Committee:
- Senate Health
- Law Section:
- Social Services Law
- Laws Affected:
- Add §365-i, rpld §364-j subs 25 & 25-a, Soc Serv L; amd §§270 & 272, add §274-a, Pub Health L
- Versions Introduced in Other Legislative Sessions:
-
2015-2016:
A9271
2017-2018: A4233
2019-S5923 (ACTIVE) - Sponsor Memo
BILL NUMBER: S5923
SPONSOR: RIVERA
TITLE OF BILL: An act to amend the social services law and the public
health law, in relation to extending the preferred drug program to medi-
caid managed care providers and offering the program to other health
plans; and to repeal certain provisions of the social services law
relating thereto
PURPOSE OR GENERAL IDEA OF BILL:
To provide the Medicaid drug benefit through utilization of the
preferred drug program (PDP) under Public Health Law Art. 2-A, rather
than through individual Medicaid managed care plan drug benefits.
SUMMARY OF SPECIFIC PROVISIONS:
The Preferred Drug Program under Public Health Law Art. 2-A would admin-
ister the drug benefit for the whole Medicaid program, including negoti-
ating rebates with drug companies seeking to have their drugs on the
preferred drug list to avoid requiring private authorization. In order
2019-S5923 (ACTIVE) - Bill Text download pdf
S T A T E O F N E W Y O R K
________________________________________________________________________
5923
2019-2020 Regular Sessions
I N S E N A T E
May 16, 2019
___________
Introduced by Sen. RIVERA -- read twice and ordered printed, and when
printed to be committed to the Committee on Health
AN ACT to amend the social services law and the public health law, in
relation to extending the preferred drug program to medicaid managed
care providers and offering the program to other health plans; and to
repeal certain provisions of the social services law relating thereto
THE PEOPLE OF THE STATE OF NEW YORK, REPRESENTED IN SENATE AND ASSEM-
BLY, DO ENACT AS FOLLOWS:
Section 1. Legislative findings. This legislature finds that the costs
of many prescription drugs in the market have been escalating unreason-
ably. The preferred drug program and the clinical drug review program
under the public health law provide effective mechanisms for assuring
access to quality, effective and safe drugs to patients at reasonable
cost. Providing prescription drugs to Medicaid managed health care
provider participants through these programs will maximize the Medicaid
program's ability to negotiate more substantial rebates with drug
manufacturers (effectively, lower prices), while protecting Medicaid
managed care provider participants. Offering non-Medicaid health plans
the opportunity to use these programs will help lower costs for those
health plans and those who pay their premiums, while protecting individ-
uals covered by those plans, and will also further increase the negoti-
ating power of the programs.
§ 2. The social services law is amended by adding a new section 365-i
to read as follows:
§ 365-I. PRESCRIPTION DRUGS IN MEDICAID MANAGED CARE PROGRAMS. 1.
DEFINITIONS. (A) THE DEFINITIONS OF TERMS IN SECTION TWO HUNDRED SEVENTY
OF THE PUBLIC HEALTH LAW SHALL APPLY TO THIS SECTION.
(B) AS USED IN THIS SECTION, UNLESS THE CONTEXT CLEARLY REQUIRES
OTHERWISE:
(I) "MANAGED CARE PROVIDER" MEANS A MANAGED CARE PROVIDER UNDER
SECTION THREE HUNDRED SIXTY-FOUR-J OF THIS ARTICLE, A MANAGED LONG TERM
EXPLANATION--Matter in ITALICS (underscored) is new; matter in brackets
[ ] is old law to be omitted.
Comments
Open Legislation is a forum for New York State legislation. All comments are subject to review and community moderation is encouraged.
Comments deemed off-topic, commercial, campaign-related, self-promotional; or that contain profanity, hate or toxic speech; or that link to sites outside of the nysenate.gov domain are not permitted, and will not be published. Attempts to intimidate and silence contributors or deliberately deceive the public, including excessive or extraneous posting/posts, or coordinated activity, are prohibited and may result in the temporary or permanent banning of the user. Comment moderation is generally performed Monday through Friday. By contributing or voting you agree to the Terms of Participation and verify you are over 13.
Create an account. An account allows you to sign petitions with a single click, officially support or oppose key legislation, and follow issues, committees, and bills that matter to you. When you create an account, you agree to this platform's terms of participation.