| Date of Action |
Assembly Actions -
Lowercase Senate Actions - UPPERCASE |
|---|---|
| Jan 03, 2024 |
referred to health |
| Feb 23, 2023 |
referred to health |
Senate Bill S5136
2023-2024 Legislative Session
Sponsored By
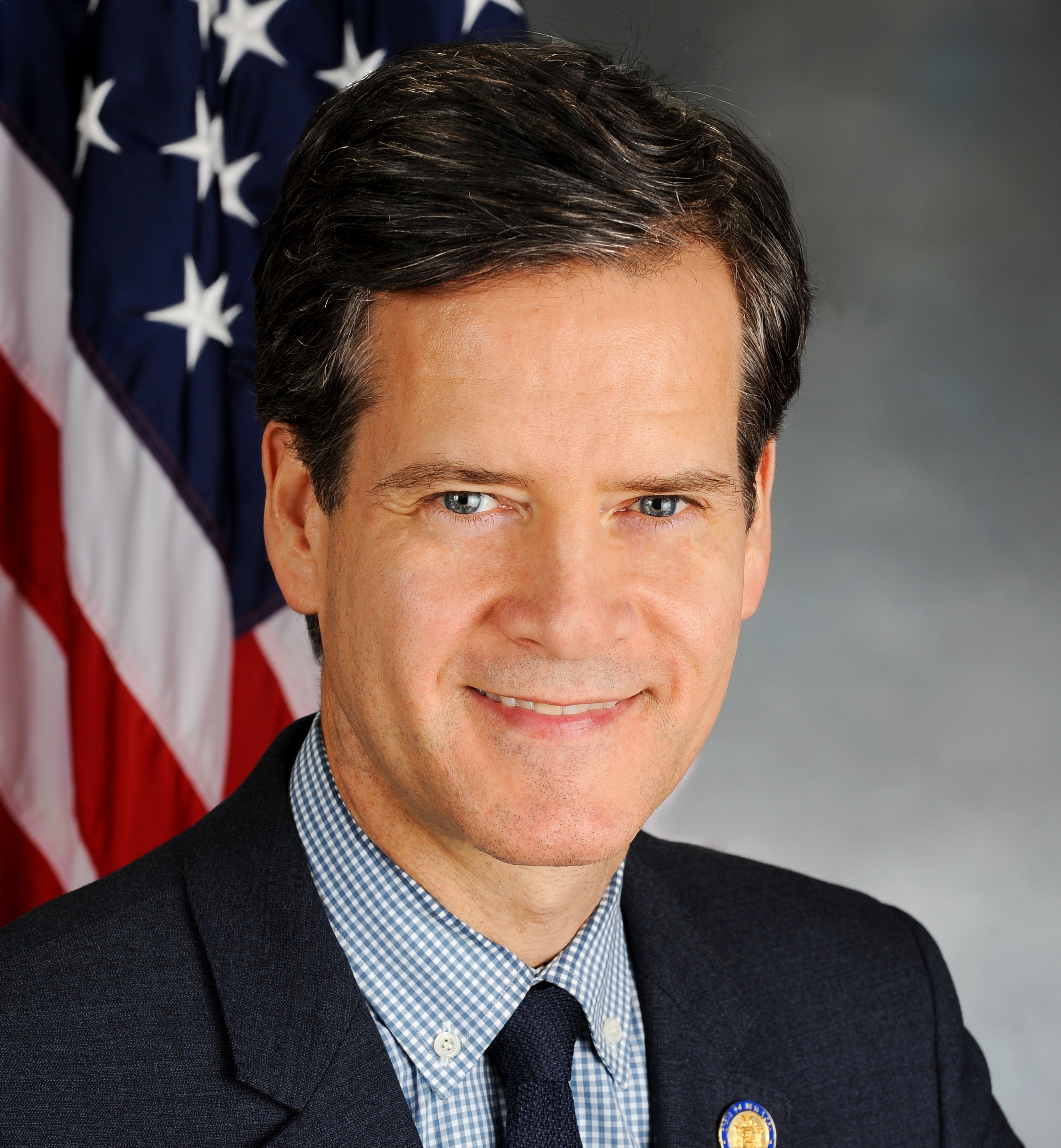
(D, WF) 33rd Senate District
Archive: Last Bill Status - In Senate Committee Health Committee
Actions
co-Sponsors
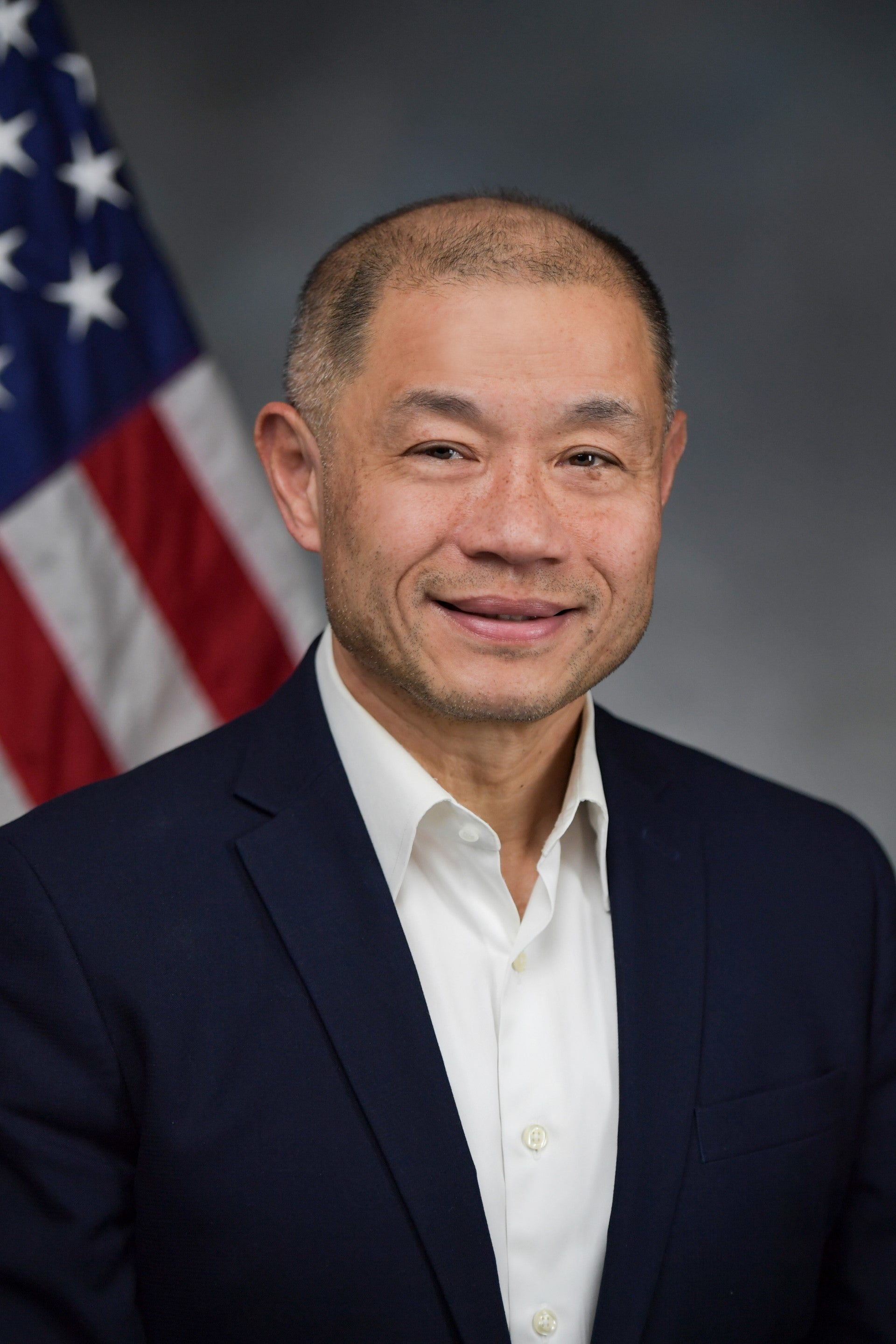
(D) 15th Senate District
(D, WF) 55th Senate District
(D) 30th Senate District
(D, WF) 56th Senate District
2023-S5136 (ACTIVE) - Details
- See Assembly Version of this Bill:
- A5911
- Current Committee:
- Senate Health
- Law Section:
- Social Services Law
- Laws Affected:
- Rpld Part FFF §§1 & 1-a, Chap 56 of 2020; amd §364-j, Soc Serv L; amd §280-a, Pub Health L
2023-S5136 (ACTIVE) - Sponsor Memo
BILL NUMBER: S5136
SPONSOR: RIVERA
TITLE OF BILL:
An act to amend the social services law and the public health law, in
relation to pharmacy services provided by managed care providers and to
repeal sections 1 and 1-a of part FFF of chapter 56 of the laws of 2020
relating to directing the department of health to remove the pharmacy
benefit from the managed care benefit package and to provide the pharma-
cy benefit under the fee for service program, in relation thereto
PURPOSE OR GENERAL IDEA OF BILL:
The purpose of this bill is to repeal the transition of the Medicaid
pharmacy benefit from managed care to fee-for-service, which would cause
unintentional harm to certain providers participating in the federal
340B program, while still maintaining protections for pharmacy oper-
ations and reducing administrative costs associated with the 340B
program.
SUMMARY OF SPECIFIC PROVISIONS:
2023-S5136 (ACTIVE) - Bill Text download pdf
S T A T E O F N E W Y O R K
________________________________________________________________________
5136
2023-2024 Regular Sessions
I N S E N A T E
February 23, 2023
___________
Introduced by Sen. RIVERA -- read twice and ordered printed, and when
printed to be committed to the Committee on Health
AN ACT to amend the social services law and the public health law, in
relation to pharmacy services provided by managed care providers and
to repeal sections 1 and 1-a of part FFF of chapter 56 of the laws of
2020 relating to directing the department of health to remove the
pharmacy benefit from the managed care benefit package and to provide
the pharmacy benefit under the fee for service program, in relation
thereto
THE PEOPLE OF THE STATE OF NEW YORK, REPRESENTED IN SENATE AND ASSEM-
BLY, DO ENACT AS FOLLOWS:
Section 1. Sections 1 and 1-a of part FFF of chapter 56 of the laws of
2020 relating to directing the department of health to remove the phar-
macy benefit from the managed care benefit package and to provide the
pharmacy benefit under the fee for service program, are REPEALED.
§ 2. Subdivision 4 of section 364-j of the social services law is
amended by adding four new paragraphs (x), (y), (z) and (aa) to read as
follows:
(X) NOTWITHSTANDING ANY PROVISION OF LAW TO THE CONTRARY, MANAGED CARE
PROVIDERS UNDER THE MEDICAL ASSISTANCE PROGRAM AND ANY PHARMACY BENEFIT
MANAGERS ACTING ON THEIR BEHALF, AS DEFINED IN SECTION TWO HUNDRED
EIGHTY-A OF THE PUBLIC HEALTH LAW, SHALL BE REQUIRED TO REIMBURSE RETAIL
PHARMACIES FOR EACH OUTPATIENT DRUG, AT THE NATIONAL AVERAGE DRUG ACQUI-
SITION COST (NADAC), OR IF NADAC PRICING IS UNAVAILABLE FOR A DRUG,
REIMBURSEMENT SHALL BE PURSUANT TO THE CURRENT BENCHMARKS UNDER FEE-FOR-
SERVICE, PLUS A TIERED PROFESSIONAL DISPENSING FEE BASED ON PRESCRIPTION
CLAIMS VOLUME TO BE DETERMINED BY THE COMMISSIONER. IN DETERMINING A
PROFESSIONAL DISPENSING FEE, THE COMMISSIONER SHALL ISSUE A SURVEY THAT
COLLECTS CLAIMS VOLUMES FROM ENROLLED PHARMACIES, AND OTHER SUCH INFOR-
MATION AS THE COMMISSIONER MAY DEEM NECESSARY TO WEIGH REGIONAL VARI-
ANCES AND OTHER FACTORS SIGNIFICANTLY IMPACTING MARKETS FROM THE PREVI-
EXPLANATION--Matter in ITALICS (underscored) is new; matter in brackets
[ ] is old law to be omitted.
LBD09373-03-3
Comments
Open Legislation is a forum for New York State legislation. All comments are subject to review and community moderation is encouraged.
Comments deemed off-topic, commercial, campaign-related, self-promotional; or that contain profanity, hate or toxic speech; or that link to sites outside of the nysenate.gov domain are not permitted, and will not be published. Attempts to intimidate and silence contributors or deliberately deceive the public, including excessive or extraneous posting/posts, or coordinated activity, are prohibited and may result in the temporary or permanent banning of the user. Comment moderation is generally performed Monday through Friday. By contributing or voting you agree to the Terms of Participation and verify you are over 13.
Create an account. An account allows you to sign petitions with a single click, officially support or oppose key legislation, and follow issues, committees, and bills that matter to you. When you create an account, you agree to this platform's terms of participation.